The Dream of Precision Medicine; The Reality of Missing Data
To understand the revolution of precision medicine, think of a library not unlike the library of Alexandria in its scope. It would contain all the robust and relevant medical data in the known world—which in this case would comprise over a million Americans—and it would be shareable with researchers and doctors. The goal? E Plurubus Unum: out of the many, and through mapping the boundaries of individual variation, we could understand the one. With such keys, we could design innovative clinical trials, devise new combinatory therapies, and broaden our understanding of drug resistant infections. We could create a platform for more accurate diagnoses, develop novel therapeutics, and make health data portable within the US healthcare system. We could unlock you.
These were the exciting possibilities discussed at the recent annual Health Data Consortium in Washington. Dr. John White, the Deputy National Coordinator for Health Information Technology told experts from around the country that the Obama administration’s Precision Medicine Initiative will combine research, technology, and policy to create a system where engaged patients will participant in shaping the new data initiative. A key aspect of this will allow patients to add such information to their electronic health records (EHRs), the current approach that healthcare professionals use to review and record a patient’s health data. Unfortunately, a major flaw in the system has been poor record keeping in individual EHRs and the challenge of moving these records from one doctor to another. “We need information to flow […] in a timely meaningful way for the right treatments to reach the right patients at the right time,” said White.
Precision medicine in theory and in practice
Dr. Chirag Patil, the Director of the Center for Neurosurgical Outcomes Research at Cedars-Sinai Medical Center, told the conference that “precision medicine is not a new idea.” He believes every good doctor individualizes patient care, and that what we are building is precision science by creating a comprehensive dataset that empowers already-practiced precision medicine. He elaborated on how he treats glioblastoma patients (a fatal brain cancer) by extracting the cancer and dividing the tissue sample between the pathologist, genomics core and cell culture specialist. Numerous studies have been published showing that cancer cells exhibit different genetic variations, and cancers may be better described by their specific gene variations rather than their organ of origin.The tissue is genetically sequenced and the data in input into a mathematical model where Dr. Patil can test how certain anti-cancer drugs could theoretically combat that specific cancer. Therapy recommendations extracted from the model could then be tested in vitro on the patient’s specific cancer grown in culture (before supplied to the patient). However, the mathematical model relies on the quality and thoroughness of reported data on current drugs. Now recall that half up to half of that trial data may not be accessible. The question is whether this process for designing and tailoring therapies for patients is scalable solution, both financially and in practice. As a surgeon, Dr. Patil has access to tangible and expendable patient tissue; but what about those patients who suffer from more complicated aliments such as bipolar and depression. How would one create a mathematical model and test therapies before entering the patient that is specific to that patient’s genetic profile or lifestyle? As conference attendee Dr. Christine Tuley, Chief Medical Officer at Health Sciences in South Carolina and Professor of Clinical Pediatrics at USC, told Sense About Science USA:
“I find myself still considering the scalability of these new frontiers in medicine—they hold such promise! There is an eagerness and hopefulness that is almost palpable among patients for this concept of precision science/medicine to lead to the next generation of breakthroughs, yet there is also a general sense that comes from the patient community that the pace of this progress is too slow. This new future of medicine and healthcare is a perfect fit for Sense About Science USA, there are many who will need a clear respected voice to provide insights—from the medical community itself that is grappling with a transformation in fundamentals of how we provide care, to the patient community—both those that are well and those that are struggling with disease, all of whom are looking for answers that are understandable and actionable.”
In a panel discussion afterwards, Sense About Science USA’s director Trevor Butterworth noted that new protocols such as Extensible Data Interchange (XDI) will solve many of the valid and pressing concerns over protecting patient health data—while enabling absolute control on what the patient decides to share. The situation we’re in now, he said, is analogous to email before the advent of SMTP (simple mail transfer protocol): different data systems cannot directly communicate with each other much like an AOL address couldn’t reach a Pine address back in 1990; XDI will allow such interchange but without having to move or transfer data anywhere. You will be able to use a link contract—a binding encrypted permission that allows you to control what is shared. This has revolutionary potential for clinical trials, Butterworth said, as—in theory—any participant in a trial anywhere will be able to give any researcher access to their data on their terms.  But, he said, the technology to do all this is about five years away. What we need to do right now was to “go back to the future” by focusing on those clinical trial results that have not been published, estimated at up to fifty percent of all the clinical trials ever conducted; and by ensuring that our current technologies for data sharing in medicine—notably clinicaltrials.gov—were supported and used. Solve the problems that are solvable now, argued Butterworth, and let technological innovation take care of the rest in due course. This wasn’t just important from a practical point of view; it was easy to get lost in the excitement of precision medicine and to forget that data privacy is a wider cultural issue—one generating increasing concern in society. No matter how much promise personalized medicine held, successful implementation would be affected by more general privacy concerns. Butterworth recalled visiting a major contract research organization for a story for the New Yorker.com, and being told that concerns about surveillance and data tracking were already leading patients in trials to worry about consenting to share such basic yet critical information as their ages. The pharmaceutical industry, he said, needed to focus now on building the kind of trust that would be essential for precision medicine to work in the future—and the best way they could do this would be by embracing the goals of the AllTrials campaign.
But, he said, the technology to do all this is about five years away. What we need to do right now was to “go back to the future” by focusing on those clinical trial results that have not been published, estimated at up to fifty percent of all the clinical trials ever conducted; and by ensuring that our current technologies for data sharing in medicine—notably clinicaltrials.gov—were supported and used. Solve the problems that are solvable now, argued Butterworth, and let technological innovation take care of the rest in due course. This wasn’t just important from a practical point of view; it was easy to get lost in the excitement of precision medicine and to forget that data privacy is a wider cultural issue—one generating increasing concern in society. No matter how much promise personalized medicine held, successful implementation would be affected by more general privacy concerns. Butterworth recalled visiting a major contract research organization for a story for the New Yorker.com, and being told that concerns about surveillance and data tracking were already leading patients in trials to worry about consenting to share such basic yet critical information as their ages. The pharmaceutical industry, he said, needed to focus now on building the kind of trust that would be essential for precision medicine to work in the future—and the best way they could do this would be by embracing the goals of the AllTrials campaign.
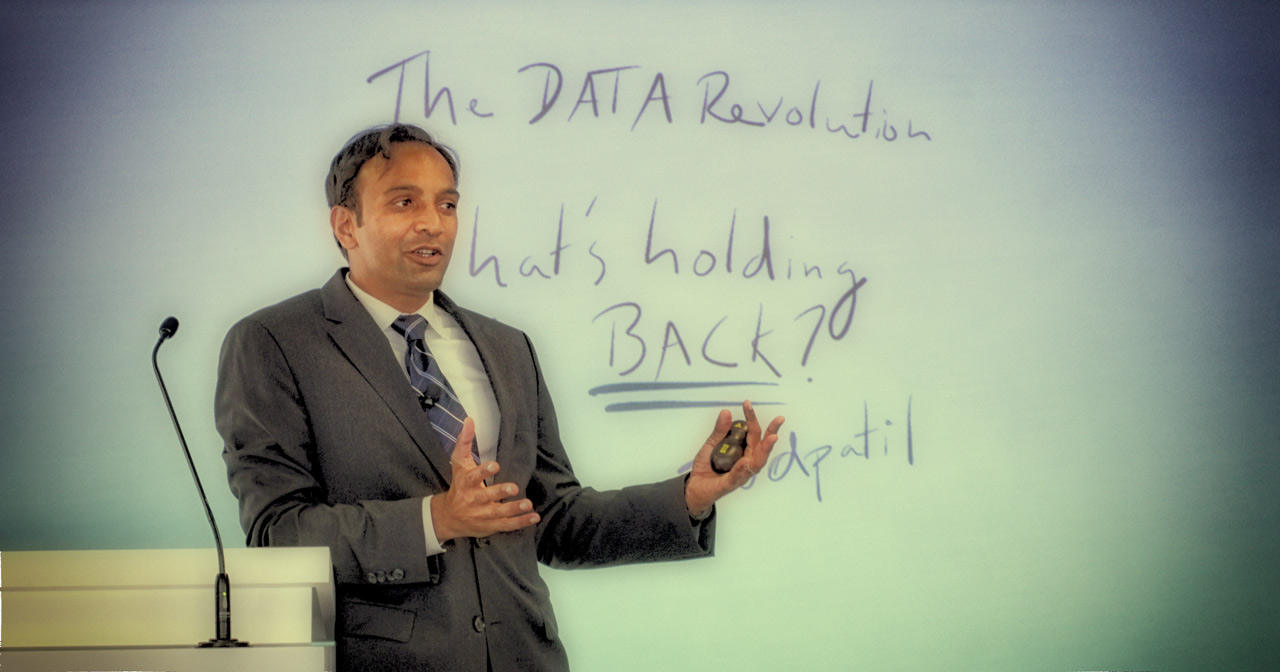
Photo credits: Top photo, U.S. Chief Data Scientist at White House Office of Science and Technology Policy, DJ Patil; bottom photo, panel discussion—Amy Chang, Digital Media and Communications Manager, Health Data Consortium.

Interesting and I hope that this dream turns into reality! Great work.
Great work ! Lot of efforts will have to take for all the data collection, interpretation and further data management for conclusion towards the target.