The Sun is Out: Risk of skin cancer in different groups

Acommon refrain about skin cancer is that it affects one in five Americans in their lifetime. Yet not all skin cancer is the same, and its impact varies tremendously according to its type. A small collection of squamous cells is a mild annoyance requiring minor surgical intervention, while deadly melanoma kills about two in fifteen people who are diagnosed. Melanoma occurs less frequently than other kinds of cancer but about one in fifty people will be affected, with some people at much higher risk than others.
Last year, more than 76,000 people were diagnosed with melanoma in the United States, according to the National Cancer Institute (NCI); more than 10,000 people died from the disease. An additional 7,000 people are diagnosed each year with non-epithelial skin cancer, a form of non-melanoma skin cancer that invades deeper tissues and carries greater risk even than melanoma; about 3,500 people are expected to die from it in 2016.
Keeping numbers in perspective is a difficult task—is the number of deaths large, in relation to the population of the United States? We look here a little more closely at the melanoma rates. Is the risk for melanoma constant, or are there ways to minimize the risk? And what is the risk for you specifically, anyway? And as sunscreen comes under some scrutiny (Does it cause infertility? Does it kill fish?) the importance of assessing these risks carefully is even higher.
Melanoma, like most cancers, has a complicated relationship to our age, body, genetic and environmental background. It can be impossible to tease out all the differences, especially because the melanoma rates are a moving target. One meta-analysis found that risk factors for melanoma included the latitude at which a study was conducted, and that latitude also correlated to sunburns. Intermittent exposure—such as a vacation at a beach or a tanning session at the salon—was riskier than chronic sun exposure, such as the amount of sun a farmer might get. Teasing out the risks from sunburn is a daunting task; our aim here has been to present the overall population-based risk and then focus in on what an individual’s risk might be depending on who that individual is.

Sunburn and sun exposure
Sunburn has long been thought to increase the risk of skin cancer, and specifically melanoma. People who have experienced sunburn are generally at higher risk than those who haven’t, though estimates about how high a risk are hard to quantify. In a meta-analysis trying to assess how much sunburn impacts risk, and whether childhood sunburn is worse than adult sunburn, the authors found that both childhood and adult burns resulted in increased risk; and that risk was seen with both typical, painful sunburn and with sunburn that results in blistering. Just as important, the risk of cutaneous melanoma was higher among those who had more sunburn, suggesting that the more unprotected sun exposure one gets, the more likely one is to get melanoma.
Questions of causality loom and have only been partially addressed in studies on sun exposure, burning, and other factors contributing to higher cancer rates. The first concern is whether sunburn serves merely as a surrogate for sun exposure. In other words, does sunburn correlate to increased risk independent of sun exposure, or is the observed relationship between sunburn and melanoma merely a reflection of greater sun exposure for people with more sensitive skin? Perhaps sun exposure, independent of sunburn, is correlated with increased risk. And in either case, does sunscreen actually make a difference?
To answer the sunscreen question as best as possible, we turn to a well-designed experiment conducted in Australia in the 1990s, in which 1,661 people ages 25 to 75 in Queensland, Australia, were randomly assigned either “daily” or “discretionary” use of sunscreen to their heads, necks and arms, over a period of four and a half years. Fifteen years later, the authors compared the melanoma rates for each group. There were twice as many people who had a “first” case of melanoma among those who did not use sunscreen regularly, compared to those who did; 11 out of the 812 sunscreen-users got melanoma, while 22 out of the 802 no-sunscreen group were diagnosed with melanoma.
The numbers were too low to reach statistical significance (p=.051), but the evidence was compelling. Among these study participants, three of the sunscreen group and 11 of the no-sunscreen group developed invasive case of melanoma, a more dangerous form of melanoma that has already penetrated deeper into the patient’s body. This difference did reach statistical significance (p=.045). Keep in mind that these p-values only indicate the probability of seeing the differences we observed in these two groups (or more extreme), under the assumption that there is no difference in their risk for melanoma. In both cases, the numbers are small but suggestive that daily sunscreen use is protective against melanoma.
Other studies suggest that sunscreen may not be protective against melanoma or perhaps even against sunburn. People buoyed by their protective sunscreen may be more likely to be burned due to carelessness. A Danish study found that using sunscreen was positively correlated with sunburn. Unfortunately, as with all observational studies, it can be impossible to isolate the underlying actions here: Is sunscreen at issue, or behaviors around it? And are people who wear more sunscreen more likely to remember sunburn (since it’s on their minds)? Are people wearing sunscreen increasing their time in the sun, or are sunbathers turning to sunscreen? We simply do not know. Similarly the relationship between melanoma and sunscreen is next to impossible to pin down retroactively.
Another meta-analysis directly investigated the question of whether sunburn or sun exposure created risk. The answer? Both. The amount of risk can’t easily be quantified because of the many methods used by the 57 articles that composed the meta-analysis. Different authors defined intermittent sun exposure differently, but the pooled group of those meeting the definition, compared to those who didn’t, indicated an increased risk of 61 percent (RR = 1.61 (95% CI: 1.31; 1.99) for those who are exposed, compared to those who are not.
However, this risk changed according to which factors were accounted for, and even which countries were included. And the risk of melanoma was greater for those who had been sunburned. Previously sunburned people were twice as likely to get melanoma (RR = 2.03; 95% CI: 1.73, 2.37) compared to those who hadn’t been. Again, various adjustments to the data had an impact on the strength of that relationship, but all but one study in the meta-analysis found increasing burns were correlated with increased melanoma.
It may be that sun exposure and sunburn cannot be entirely separated, however there is evidence that broad spectrum, high SPF sunscreen makes a difference. It also may be that sun exposure is more harmful to people with some types of skin than others; many questions remain even as there is strong evidence that sun exposure and sunburn have a causal influence on melanoma cancer. The evidence that sun is doing the damage, possibly through several mechanisms, is widely accepted, as is the claim that sunscreen protects against exposure.
Men, women and children: some surprising comparisons
Like all forms of cancer, skin cancer, and deadly melanoma and non-epithelial cancer in particular, have a complicated and multi-faceted genesis, but it often doesn’t get the attention it deserves.
While breast cancer stands as the most common form of cancer for women (excluding basal and squamous skin cancer), the rates of dying once diagnosed with cancer are similar to those of melanoma. The estimated number of new female breast cancer cases in the U.S. for 2016 is 246,660, while the estimated number of new female melanoma cancer cases (melanoma and other non-epithelial skin cancer) is comparatively small, at 29,510. But after five years, about 10.3 percent of people diagnosed will die from breast cancer, and 8.5 percent of those diagnosed with melanoma will die from it. If we include non-epithelial skin cancers, a rare form of skin cancer even more deadly than melanoma, the total for women goes to 31,860. The expected deaths in 2016 from these two forms of skin cancer are 4,320, which amounts to about 13.5 percent of the number of diagnoses for the same year. In comparison, 40,450 women are expected to die in 2016 from breast cancer, about 16.4 percent of the number of diagnoses.
Women are almost 50 percent more likely to get melanoma than to get ovarian cancer, though ovarian cancer is far deadlier, with only 46.2 percent of women surviving 5 years after diagnosis.
When men and women are grouped together, the estimated 2016 number of deadly skin cancers is 83,510, which is significantly larger than the number for leukemia (at 60,140), though leukemia patients are much more likely to die of the disease.
Melanoma’s death rate in the whole population (2.7 per 100,000 men and women) is a fraction of the rate for female breast cancer (21.5 per 100,000 women), yet death from skin cancer is 40 percent higher than oral cancer, higher than myeloma, and more than half the rate of leukemia.
Melanoma strikes children, too, although at a low rate: The incidence for kids and teens under 20 is about 5 or 6 cases of melanoma per million people. The incidence for kids ages 0-14 is only 2 in a million. And the rates for kids are trending downward, possibly due to more aggressive use of sunscreen by parents.
What does the future hold? Melanoma rate changes
Melanoma is also on the rise, and the trend has resulted in an enormous 50 percent increase in the rate over the past 20 years. In 1992, there were 14.1 cases per 100,000 people in the United States, and in 2013 (the last year for which data is available), the rate was 21.5 per 100,000. The good news, peering out from the depressing upward trend in incidence rates is that death rates appear stable since about 2003, with approximately 2.7 deaths per 100,000 people. In other words, getting melanoma is an increasing problem (unless we could attribute rising rates to more aggressive diagnoses) but dying from it has been kept in check. This SEER graph shows the increasing diagnosis trend for melanoma but the fairly constant death rate in the population.

At least in theory, the increase in diagnosis could indicate aggressive diagnoses of cases that may not have otherwise led to death. More likely, the chart is showing an encouraging improvement in treating melanoma. Among those who get melanoma, the death rate has actually gone down, from about 19 percent of those who got melanoma in the early 90s, to about 12 percent currently. Right now, more than 90 percent of those who receive a diagnosis of melanoma will survive more than five years.
The rapidly rising incidence over the past 30 years may have an end in sight: As the American Cancer Society noted, “the past 5 years of data indicate that rates are declining or plateauing among those younger than 50. For example, from 2008 to 2012, incidence rates declined by about 3% per year in both men and women ages 20-29. In contrast, among adults 50 and older, the incidence rate has increased by 2.6% per year since 1996.”
In other words, rates are declining for people under 30 over the past few years, suggesting that this younger group has been more careful to protect itself. In contrast, the rates for middle-aged people are increasing, and have been increasing for 20 years. It may be that earlier sun exposure has caught up with them, with a delayed effect responsible for a delayed melanoma rate increase. It may be that increased sunscreen and sun-protecting clothing is resulting in reduced rates, an encouraging sign for melanoma rates looking forward as this younger group ages.
The Centers for Disease Control projects that incidence rates will continue to increase through 2019 for both male and female white U.S. residents, and then plateau, barring significant interventions creating cultural shifts to avoid sun exposure and to use sunscreen and clothing to protect against the sun.
A day at the beach
So what might a day at the beach do to your skin? This question is hard to answer, in part because little research directly relates the number of hours of exposure to the sun and getting skin cancer.
If the day at the beach results in sunburn, however, we can at least get some ranges for the increased risk.
Kids who have had sunburn have about 90 percent increased odds of getting melanoma in their lives, compared to kids who have never had sunburn, according to this meta-analysis of 51 studies. Adolescents who have ever been burned have a 63 percent increased odds of developing melanoma, and adults have a 44 percent increased chance. Generally speaking blistering sunburns are associated with greater risk.
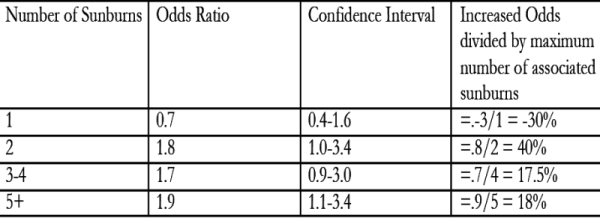
Increased number of sunburns also resulted in increased risk, though different studies had different numbers reported, suggesting high variation in the outcome (or large error in sunburn reporting). A general rule of thumb seems to be about a 10 to 20 percent increased odds for each sunburn. For example, in one study on Caucasians in the US, the authors compared the odds of melanoma among those having had various numbers of sunburn over the course of their lifetimes, to those who had not. The results are listed in the table below:

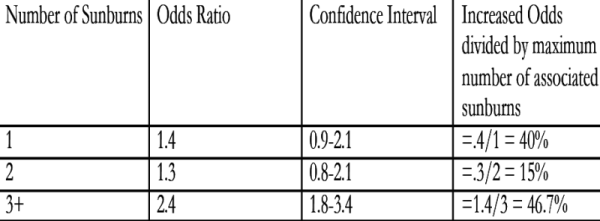
A 1980s study on white women in the U.S. made a similar comparison, this time using blistering burns in adolescence:
And yet another U.S. study looked at childhood sunburns and subsequent melanoma diagnoses, finding these odds ratios:
The high level of variation in the data suggests the difficulties in conducting this research, but the direction of the results singularly points toward increased risk.
As we mentioned, intermittent sun exposure is associated with a 61 percent increase in melanoma, but quantifying “intermittent” is a challenge, since different studies use different meanings, and some are more precise than others. One protected day (with sunscreen and/or sun-proof clothing and/or shady environment) at the beach may not be adding a big risk for melanoma, and it’s almost certainly less risk than an unprotected day at the beach.
What can sunscreen do to mitigate these effects? Estimates range for how well melanoma can be driven down by the consistent use of sunscreen. The well-designed Australian study (Green, et al.) mentioned above certainly found a reduction in melanoma among those using sunscreen, but the percentage of reduction (50 percent in this case) may be unreliable due to small numbers. Other studies also support the conclusion that sunscreen reduces the risk of melanoma, such as a study on Canadian children and the development of nevi (moles or beauty marks).
The Environmental Working Group (EWG) points to research suggesting that sunscreen increases the risk of melanoma, but others suggest that a noted increased risk may be plagued by confounders and misleading correlations. In particular, people at high risk of melanoma may also be more likely to use sunscreen —resulting in higher melanoma rates among those who use sunscreen. There are also questions about the causal pathway: if using sunscreen results in people sunbathing longer, then should sunscreen be blamed for the ensuing skin damage and cancer risk, or should people’s decisions?
Skin cancer development resulting from sun damage takes many years to develop, making efforts to identify a benefit of sunscreen difficult to isolate. The best evidence overall suggests that regular sunscreen makes a difference in melanoma rates, if it is used to reduce the risk of sunburns. While the Green study established sunscreen’s efficacy in fending off damaging UV rays and reducing the risk of melanoma in the context of everyday life, sunscreen should not be used to justify increased sun exposure. The question of whether behaviors change due to the existence of sunscreens carries important consequences for any public health campaign: clothing and staying out of the sun is a greater defense than sunscreen.
Skin type
Protection against melanoma comes largely in the form of skin type. The Fitzpatrick Skin Type scale was developed to override simple notions of race, and provides a starting point to assess one’s risk. But not only fair-skinned people are susceptible to melanoma; those who have a lot of moles or other growths on their skin are also at greater risk.
Data on race may shed some light on the different risks by skin type, however. The incidence rate of skin cancer in 2011 was 19.7 per 100,000 U.S. people, according to the CDC, but this varied tremendously by race, a surrogate for skin type. As many as 24.6 per 100,000 Non-Hispanic Whites (NHW) were diagnosed with melanoma in 2011, compared to 4.2 out of 100,000 among Hispanic Whites, 4.3 among Hispanics generally, 4.3 per 100,000 among American Indians/Alaskan natives, 1.0 out of 100,000 Blacks, and 1.3 out of 100,000 Asian/Pacific Islanders.
While melanoma may seem like a “white” problem, death rates adversely affect other groups more than whites. While the incidence of melanoma is almost 25 times higher for Non-Hispanic Whites than for Blacks (24.6/1.0 = 24.6), the rate of death was just 8.5 times higher. White non-Hispanics died from melanoma at a rate of 3.4 per 100,000 while Blacks died from it at a rate of 0.4 per 100,000 (3.4/.4=8.5). Hispanics also have a proportionally higher death rate. The melanoma incidence among Non-Hispanic Whites is about six times the size as that for Hispanics (24.6/4.3 = 5.7), yet the death rate is only four times as large (3.4/.8 = 4.25). Among diagnosed cases, Blacks are more likely to die of melanoma than Whites or Hispanics. One cause may be overall poorer health care, but many dermatologists also point to the reduced recognition (and search) for melanoma among people with low-risk skin types.
Skin type may not be the only factor in lower rates. A recent report compares the rate of melanoma in the U.S. Hispanic population to the Non-Hispanic White population in California. The lower melanoma rate cannot be explained by differences in skin type, large moles, hair color, or even sunburn rate. Sun exposure, and genetics both remain unknown in impact. At the same time, the authors attribute increasing melanoma rates among Hispanics to an increasing number of sunburns.
Behavior resulting from skin type may also be a factor. People who can’t tan are more likely to avoid the sun or to use sunscreen, with the result that we may be under-estimating the risk associated with sun exposure. The Gandini study’s analysis of intermittent sun exposure “suggested that if we do not take into account phenotype and phototype for adjustment of the estimates we will obtain RRs that are lower not because of the sun effect, but probably because people with sensitive skin do not try to tan to the same extent.” In other words, people who are more likely to burn – typically fair skin types – tend to stay out of the sun (decreasing sun exposure), while those who more easily tan tend to stay in the sun (increasing sun exposure). The “average” exposure doesn’t take this into account, and the corresponding melanoma rate is lower than it would be if people were acting independent of their skin type.
And the take away?
Sunburn, sun exposure, and tanning beds are all convicted culprits for melanoma risk. And for avoiding sunburn, our choices are limited: stay out of the sun, wear sun-blocking clothes, and apply sunscreen. Your risk is higher if you are white and non-Hispanic, older, and male. On the other hand, even if you are a young black female, careful attention to any possible skin abnormalities could save your life.
Melanoma steals an average of 17.1 years of someone’s life. With more than 10,000 people to die in the U.S. alone, the stakes are high. While genetics and randomness play a role, evidence is strong that sun exposure and sunburn both play a role in the development of melanoma. Staying out of the sun (especially in peak hours), wearing protective clothing, and wearing sunscreen are all effective ways to minimize burning and melanoma risk.
Please note that this is a forum for statisticians and mathematicians to critically evaluate the design and statistical methods used in studies. The subjects (products, procedures, treatments, etc.) of the studies being evaluated are neither endorsed nor rejected by Sense About Science USA. We encourage readers to use these articles as a starting point to discuss better study design and statistical analysis. While we strive for factual accuracy in these posts, they should not be considered journalistic works, but rather pieces of academic writing.


I believe there may be a typo in this article. “Whites died from melanoma at a rate of 3.1 per 100,000 while Blacks died from it at a rate of 0.4 per 100,000 (3.4/.4=8.5).” Is the rate of death caused by melanoma for whites 3.1 or 3.4 per 100,000?
Thank you Karl for noticing our error. We have made the correction. Thank you again.
Going to beach next week with teenagers. Thank you for the information!